Category: Uncategorized
Coronavirus 19 Info and Guidelines
Thank you to Dr. Allison Edwards from KC DPC for her work on a majority of this information.

Good Afternoon,
We are reaching out because we know this is a confusing and anxiety provoking time for many people. As you are likely aware, Massachusetts residents have tested positive for COVID-19 (the illness caused by the novel Coronavirus) and we expect more cases to be identified as testing availability expands over the coming days to weeks. As of earlier today there are a total of 95 presumptive and confirmed cases of coronavirus in the state. Most of the these patients will do very well and will not require hospital level of care.
As your physicians, we are committed to staying up to date on developments and changes, so that we can provide you with the most accurate and timely information possible. We are routinely reviewing updates from the Massachusetts Department of Public Health (https://www.mass.gov/orgs/department-of-public-health) and the CDC (www.CDC.gov). If you have questions or concerns, we strongly urge you to visit and utilize these resources. We do not recommend you get your information from social media.
This is not a time to panic, but we do all need to institute some changes in our day to day lives to try to slow the spread of the virus. Yes, it may be inconvenient, but it is necessary. We may not be able to prevent a large portion of the population from getting this infection, and the majority of people who are infected will do just fine. However, it is very important that we slow the spread so that huge numbers of people are not infected at the same time, which would overwhelm our hospitals’ ability to care for the segment of people who need hospital level care due to severe illness. We ask that everyone practice “social-distancing” and avoid non-essential large gatherings or unnecessary travel, wash your hands frequently, avoid touching your face and stay home if you have a fever or cough. This is the best way for us to ensure that there will be adequate health care resources for folks who do get very ill from the virus.
At Gold Direct Care we are fully committed to caring for our patients in the most evidence-based, safest capacity possible. We want to make sure that you know how we plan to serve you as COVID-19 spreads through our community, so we’ve put together the following information to explain what you can expect from us over the next few weeks to months.
As of today, March 12, we are asking those with respiratory symptoms (cough, shortness of breath, wheezing) and/or fever to first call the office (781-842-3961) or text message your physician. DO NOT walk-in to the office without first calling. If you walk-in you are potentially putting our staff and other patients at risk unnecessarily. We will reach out to you for more information and determine the best way and place to evaluate you. If you have a regularly scheduled visit for a routine, non-urgent issue and you want to cancel in light of current events, please call the office and Lauren will reschedule you. Many issues can be handled over the phone, so we can always arrange a phone-visit between you and your doctor. In addition, no patients will be given an appointment without providing a brief reason for the visit. This helps us from being surprised by someone’s symptoms. Please do not “back-door” us and say you are coming in for a benign reason when really you have respiratory symptoms that should be handled as stated above. When in doubt, call the office and we will triage you appropriately.
The key points of the triage system we have put in place to keep everyone safe are as follows:
• If you have mild, isolated, upper respiratory symptoms (runny nose, nasal congestion, post-nasal drip, sore throat), but NO fever or cough, and have NOTbeen in close contact (within 6ft for at least 15 minutes) with someone diagnosed with COVID-19, nor recently returned from travel to a high transmission country (China, Iran, Italy, South Korea and Japan) or the Northwest US, we will recommend home care and that you not come in for an in-person visit. You are always welcome to schedule a phone visit with Dr. Mancini or Dr. Gold to talk through things.
• If you have lower respiratory symptoms (deep cough or shortness of breath) and/or fever your physician will recommend a telephone visit to ascertain if an in-person visit is warranted.
• If we determine that you need an in-person visit, the visit will occur in your vehicle in the parking lot of our clinic so as to prevent potential spread and exposure to others in the office. While this is not how we usually do things, it’s the most effective way to prevent the spread in the clinic.
• If you have severe symptoms, we will likely refer you directly to a hospital.
• Currently, we do not have the COVID-19 test kits in our office. All testing as of today is still being done through the Mass Department of Health. We are working with our lab vendor to confirm the exact specifics of when commercial testing will be available. When testing becomes more readily available we will continue to work with the Mass Department of Health and the CDC to determine who needs testing. We will not be recommending testing for just anyone with symptoms of respiratory infection; we will make this decision on a case-by-case basis using sound medical evidence and our clinical judgement.
I cannot be more explicit than this: if our staff comes into contact with someone who is symptomatic and positive for COVID-19, we may be required to be in quarantine for 14 days. As we are a small office, this may lead to a situation where we will have to close for all in-person interactions for up to (and potentially longer than) a 14-day period. If this were to occur, we would attempt to still offer telephone triage and telemedicine visits.
We are taking an abundance of caution by putting these guidelines in place to prevent the spread of this illness to the most vulnerable around us. We appreciate your understanding, patience, and effort to keep everyone in the community healthy as we all see our routines upended a bit by this virus.
Don’t hesitate to ask questions or reach out.
Carmela Mancini, DO and Jeffrey Gold, MD
For additional information please visit:
https://www.cdc.gov/coronavirus/2019-ncov/index.html
https://www.mass.gov/resource/information-on-the-outbreak-of-coronavirus-disease-2019-covid-19
Updated Testing Guidelines for More Information
Our Unhealthy Addiction to Health Insurance

Whenever I give a talk about healthcare, I ask the audience, “What is the worst addiction problem we have in the United States?”
The answers are typically the same and all are good guesses – alcohol, tobacco, opiates, and sugar are most frequently cited. I agree these are all terrible addictions that need to be addressed but, in my opinion, the worst addiction in America right now is to health insurance.
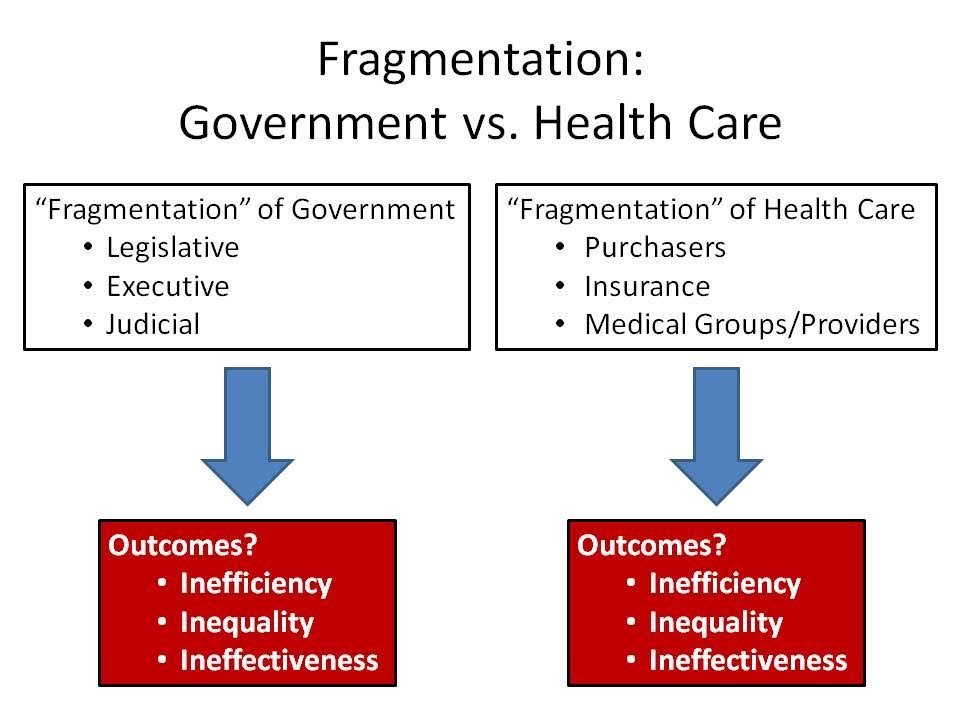
That answer usually draws a stunned or shocked silence from the audience but the numbers bear it out. The chart below shows the staggering costs American spent on healthcare in 2017. Please remember, these figures are in billions of dollars, so $2,961 spent on “personal health care” represents $2.9 trillion(!).
What is most shocking about these numbers is not just the high spend but the lack of value delivered in return. As a primary care physician who has practiced within the insurance-based system and now outside of it, I can tell you Americans are paying Porsche prices for Yugo performance.
The typical American experience in seeking healthcare is not good. There are often long waiting times for appointments (usually which could have been cleared up in an email or phone call), brief interactions with an actual doctor, high co-pays and deductibles, long waits at the office, a crushing amount of paperwork, and a stunning lack of communication. Does this fit into a description of “Porsche value”— especially when one gets the mystery, indecipherable bill for services weeks later?
The main mistake that we have succumbed to as a society is that we have deviated from the original intent of health insurance. The true purpose of health insurance was to protect people against financial ruin in the event of an unexpected, major occurrence – just like car insurance, life insurance, and homeowner’s insurance. But things got murky when people were indoctrinated into the belief that good health insurance should “cover everything” because “everything in healthcare is expensive.”
The irony is that, because of this mistake the “insurance” has become more expensive to the point it is unaffordable to many, and even those that can afford the premiums struggle to put money aside to cover the huge deductibles and coinsurance. Read yesterday’s article from Bloomberg Employer Based Health Insurance Costs over $20,000
The system got messed up when health insurance stopped being a form of insurance and instead became a default payment system. The dialogue below is an actual discussion I had this past year with a patient about lab tests.
Me: “Those lab tests will be 20 dollars cash through our pricing.”
Patient: “What will it be if I bill through insurance?”
Me: “We can send it to a hospital who will bill insurance but if you are on a high deductible plan I have no idea what your out of pocket will be, but I can guarantee it will be more than 20 dollars.”
Patient: “Ok, well let’s use insurance.”
Me: “You do understand part of the reason insurance is so expensive is because we use it as a payment model rather than insurance?”
Patient: “Well I pay a lot for my insurance so I want to use it.”
Me: *HEAD EXPLODES!!!*
(FYI- labs ended up being around 400 through insurance due to deductible)
The definition of addiction is “a psychological and physical inability to stop consuming a chemical, drug, activity, or substance, even though it is causing psychological and physical harm.” It’s discussions like these that make me assert that we are addicted to health insurance. This patient simply could not imagine not using their insurance for a simple procedure and, in so doing, drove up the prices unnecessarily for everyone. By doing this, we as a society, have let this addiction consume us, our paychecks, and our savings for our children and grandchildren. And we keep doing it because our brains tell us there is no other way.
The chart below illustrates the spiraling costs of our health insurance as payment system addiction:
One of the health insurance benefits experts I work with is correct when he says “Today’s claim is tomorrow’s premium, copay or deductible.”
Unfortunately, the hardest part of treating addiction to any substance or belief is that denial is a major part of the disease. In order to fully treat addiction successfully, the addict has to accept that they are an addict and want to get better. Once that happens you just have to ask for help and there are resources available.
This country needs help as 20% of our GDP is on health insurance and the costs of care. It is up to us as a society to fix this as we are all patients and deserve better. We deserve high quality care when we are suffering from an insurable event and should be protected from financial ruin in such cases. We also deserve transparent pricing and quality assurance.
Above all, we deserve a system with a working payment system and to stop using insurance beyond its intended purpose. Simply stated, we must break our unhealthy addiction to health insurance. I am starting a support group called AHIAA- American Health Insurance Addicts Anonymous (ironically HIAA is already being used by you guessed it….Health Insurers Association of America). As the founding member, I am willing to admit that I too am a health insurance addict, but am now in recovery. The process of recovery has not been easy, but it has been the most rewarding process of my life. This group is established to help you through this process so please join me so we can let the healing begin.
A Leap of Truth

This is dedicated to all of those on the precipice of choosing between your norm versus your actual truth. Not who you project but who you are when no one else is looking.
People often use the term “Leap of Faith” in their motivational language. Wikipedia defines a leap of faith as “an act of believing in or attempting something whose existence or outcome cannot be proved.”
Well I would like to coin a new term- a Leap of Truth. This is an act of believing in or attempting something whose existence or outcome can be or may already be proven, but one is too damn scared to admit it and step toward it. People often ask me what led me to take such a huge risk by leaving a very well paying job as a primary care physician working for one of the “best” hospital systems in the country. The answer is very simple- I took a leap of truth. I knew from the moment I filled out a coding/billing form in my residency clinic after seeing ten patients in one half-day session that this type of primary care medicine was not going to be my truth. For nine to ten years or so I struggled to put my truth into words- never mind being close to putting it into action. I could not even define it…yet. I just knew that 10 minute visit, impersonal assembly line medicine was not going to fit in the definition. I knew that spending a majority of my day trying to prove my worth to some 3rd party insurer or government agency was not going to be part of it either. I just wanted to do what I dedicated my education and life to- taking care of my patients to the best of my ability. Everything else was just useless.
So one winter night in December 2013 I was sitting on my iPad trying to figure out Twitter. After being on there for ten minutes or so, someone I followed retweeted a tweet from Dr. Josh Umbehr at AtlasMD in Wichita KS. It read something like this: “Imitrex injection for migraines 200 and something dollars in local ER. $9.10 in our clinic. #DPC” So I said to myself “what the hell is DPC and why I have I never heard of it?” Within 5 minutes I hit reply all and asked exactly that. Within minutes Josh messaged back and said he would be happy to set up a call so that I could learn more. So that next night I sat on a call with him and realized I was getting closer to defining my truth. My truth was and is Direct Primary Care. After researching the model and the labyrinth that we call American health policy for almost a year, I knew that I had to leave my norm and take a Leap of Truth.
Of course I had a lot of doubters, naysayers, skeptics and flat-out demoralizers tell me I was going to fail. Some of my favorites were “This isn’t Kansas…this is Massachusetts” and “This will never work in Massachusetts.” My all time favorite was when i told an elderly patient- one who had just switched to me after his prior doctor of 20 or so years had retired- that I too was leaving. As an employed doctor I was not allowed to do this, but I felt that it was the appropriate and right thing to tell him given his age and uncertainty in regards to his future care. So I explained the model of DPC and told him he was more than welcome to come with me if he so desired. His response upon learning I wanted to work for cash rather than government/insurers was “what are you some kind of greedy Jew or something?” You can not make this stuff up. My response was with a chuckle as I said “yeah I guess if you believe taking the biggest professional risk of my life and putting myself into a mountain of debt to do it defines a greedy Jew, then yeah I am a greedy Jew through and through and proud of it.” Needless to say, but this kind gentleman among many others did not come with me to my new practice. However, I persisted walking through the mire because I knew in my heart it was the right thing, regardless of what others had to say.
Those months from April of 2014 to December 2014 were some of the hardest months of my life. I was basically working two jobs. I was seeing a full load of patients act my old job and meanwhile trying to build a new practice. God only knows what my blood pressure was during those months, but I look back with not one regret. Sometimes doing the right thing is just really freakin hard, but once you find your truth you will find that there is nothing more comfortable….not even the norm you have grown so accustomed to.
My favorite television show of all time is Lost. Yes, some people hated it and some people loved it, but few were in between. The irony of this is that the whole series was really about the “in-between”- science vs faith, reality vs destiny, life vs death. It wasn’t about polar bears being on a tropical island. I have attached a video clip that shows the ongoing debate on the show between Jack Shephard as a man of science and John Locke as a man of faith. (Sorry for the length and ad that pops up in the middle.) So I guess the message here is that there is something between faith and science and between life and death, but it does not have to be a painful purgatory. It can be a truth in which you find peace. Do not settle for being a slave or pawn to the “system”. You put yourself through college, medical school, residency, debt, etc etc. When you think about the doctor you are vs the doctor you hoped to be you may realize that the truth is somewhere in the middle. So stop looking at DPC or some other career change as a Leap of Faith, but look at it rather as a Leap of Truth- your truth and only yours. No one can take that away from you no matter how hard they may try.
To Teach Is To Learn
Last week I was notified of an incredible honor. I received a citation of excellence in teaching along with 11 other clinical faculty in Family Medicine by the Tufts University School of Medicine 3rd year students. I am pretty sure this recognition does not come with a check, a free car, or a safari adventure but it means a heck of a lot more to me than any of those items. I would not be a physician today without the many incredible teachers I have had- from kindergarten through high school, college, medical school, residency, and clinical practice. There have been a few duds along the way, and not because they were not knowledgable, but moreso because they just seemed disengaged and unhappy teaching. Sadly a few of these duds were in medical school and unfortunately they had no idea the negative influence they had on me. One of them actually drove me away from the field of medicine that I was originally interested in pursuing. So I promised myself back then that I would never treat students that way if I ever had the opportunity to teach. I have only strived to have a positive influence on my students regardless of the field of medicine they choose. And now, by exposing them to Direct Primary Care, I hope they might realize that there is a future in primary care besides the current option of being an employed physician. However , what I did not realize when I first started teaching about ten years ago, was the incredible influence they would have on me.
Over the years, my students have reminded me of why I chose to pursue a career in medicine in the first place- particularly primary care. I see their thirst for knowledge, their drive to try to know everything, their passion to care for people, and their desire to impress me. I often chuckle on the inside when I give them a project or something to look up and they think its just a routine assignment I have given them, when in reality, it is solely so I can learn a new topic/disease or relearn an old topic/disease I have not seen in years. They keep me on my toes and challenge me to be a better educator, doctor, and person in general. They make me realize how under-appreciated primary care is as 6 week rotations do not even scratch the surface of the knowledge base that is needed to do this job well. One of the joys of medicine is that every day is a learning experience, and my students just enhance it and make it that much more enjoyable.
So, as my children finish 1st grade today (with perfect report cards I may add) I thought it would be apropos to write something that shows my appreciation for all the teachers out there, and for the students that remind us teachers that we too are still all students.
PS. Thank you to Tufts Medical School for allowing me to teach and for this incredible honor.
While Congress Fiddles, Patients Lose Patience
Published in the Boston Business Journal April 7, 2017:
The longer Republicans debate and dissect the Affordable Care Act, the more people are turning to Direct Primary Care (DPC) physicians. Unlike the recently proposed American Health Care Act — and the Affordable Care Act it is seeking to replace — direct primary care is both affordable and easy to understand.
The rising popularity of DPC practices in Massachusetts and in more than half the states where it is being practiced is in stark contrast to the utter confusion and fear that has ensued since Congress and White House set out to repeal Obamacare. A health care system once focused on prevention has given way to expensive intervention and specialty care. Experts disagree on how to fix our health care system, but it is well understood that what has been driving up the cost of health care are prescription drugs, overutilization of our hospital emergency rooms for non-emergency primary care, escalating prices for medical procedures, and unnecessary diagnostic tests. What patients — and doctors — need from our health care system is simplicity. Think of how we use car insurance to protect us from personal injury and car damage — not for the replacement of tires or windshield-wiper blades. We shouldn’t use health insurance for routine primary care.
Rebuilding the primary care foundation of our health care system won’t fix all of what is ailing health care, but it would reset a system that now largely benefits the insurance industry and pharmaceutical companies. A study by the health policy journal Health Affairs found that a direct primary care practice they studied was nearly half the cost to the patient when they purchased a lower-premium, higher-deductible insurance plan. A 53-year-old man who would have paid $11,068 for a one-year $1,000 deductible plan instead bought a higher-deductible plan and cut his health care costs by more than $4,000 annually — and he actually spent more time with his physician.
During the course of an appointment that is typically an hour or longer, DPC physicians can figure out why a patient hasn’t been sleeping rather than just writing them a prescription and dashing off to the next 12- minute appointment. We get to know our patients, their diet, whether they are exercising. That consultative relationship is critical to prevention of future and expensive illnesses such as heart disease, cancer and diabetes. Direct primary care physicians aren’t necessarily better doctors — we just spend the time that it takes to be a good doctor and actually listen to our patients. But you can’t fix what you don’t have the time to see or hear.
Day of Atonement
So today the Jewish religion celebrates the holiday of Yom Kippur. Yom Kippur for those who do not know is the most solemn and second only to the Sabbath as the holiest day of the year in Judaism. Its central themes are atonement and repentance. Jewish people traditionally observe this holy day with an approximate 25-hour period of fasting and intensive prayer, often spending most of the day in synagogue services. (This is referenced from Wikipedia.) Now, I was raised Jewish and consider myself to be a good Jew even though I may not go to temple today (or ever for that matter) or fast. To me, religion is more about how we treat each other than whether or not we have good attendance at temple/church or regardless of whether you stop eating for a day. I would also like to put a different wording to “atoning for sins or repentance.” I think the best way to look a this day is no different than how we should look at any day of our lives- as a constant learning process.
The best part of being a primary care physician, especially now that I have much more time to spend with patients, is that I really get to see people at their best and worst. I get to deeply learn about the human condition. And as a fellow human, I realize that we all have done and/or said things that we are not proud of. None of us are perfect nor will we ever be. Making mistakes is part of the learning process, and yes some are worse than others, but if we examine them and learn from them we can all grow and become a better person as a result of it. Right now in society there is a lot of rancor and venom being spread around. There is a lot of personal, internal unhappiness being projected or displaced onto others. When this happens, the cycle just repeats and repeats itself and the end result is no one ever heals- neither the person who was hurt nor the person that caused the hurt. We end up just hurting ourselves even more.
So take today- Yom Kippur- and make it and every day a “learning day”. Take the time to reflect about how you can change for the better and apologize to yourself for the mistakes you have made because until you forgive yourself, the people you have hurt won’t be able to feel the sincerity of the apology. I have always said we can only change ourselves and how we respond to people, not people. That change has to come from within. One of my favorite educators was Dr. Aaron Lazare MD who, may he rest in peace, was Dean of UMass Medical School when I was enrolled there. He was a psychiatrist and was one of the kindest people I have ever met. He wrote an incredible book called “On Apology” which spoke to how important an apology can be in life and in medicine. Here is a great quote from it:
“One of the most profound human interactions is the offering and accepting of apologies. Apologies have the power to heal humiliations and grudges, remove the desire for vengeance, and generate forgiveness on the part of the offended parties. For the offender, they can diminish the fear of retaliation and relieve the guilt and shame that can grip the mind with a persistence and tenacity that are hard to ignore.The result of the apology process, ideally, is the reconciliation and restoration of broken relationships.”
So realize we are all human….and we all screw up, but…we can apologize to ourselves so that we can heal from within and then…help others do the same.
Gut Yontiff
Defragmentation of Care- PCP and Specialist Combined Visit ( A Medical Students Take)
When was the last time your PCP accompanied you to a specialist visit? Never? Same here. That’s actually not entirely surprising in today’s healthcare environment, given the demands placed on healthcare providers and primary care physicians in particular. But last week, I had the opportunity to be a part of such a visit.
I’m a medical student on my family medicine clerkship with Dr. Gold, and on his schedule this day was a cardiology visit for one of our 78 year-old patients. In the afternoon, we drove to meet her at the cardiologist’s office. She had recently had an episode of atrial fibrillation picked up by her pacemaker, and at this appointment, we would discuss the possibility of starting her on blood thinners. The cardiologist thoroughly explained the algorithms that guide decision-making for the treatment of new a-fib, along with the risks and benefits of blood thinners. He concluded by saying that, while he slightly favored starting the medication, he would leave the decision to our patient. As she took a moment to take in this information, her eyes began to well up. Amidst her tears, she explained that having to add yet another medication to her regimen or the thought of a stroke or going into a-fib again or bleeding from a fall was all too overwhelming to process.
The situation was complicated further by our patient’s chronic pain, which she experiences as a burning sensation across her lower chest. It has been treated with varying success for many years, and she was soon visiting a pain clinic for further assessment. So how was she to decide given these circumstances? The cardiologist offered expertise focused on giving her the best possible care for her cardiovascular health and went on to reassure her that the pain was not cardiac in origin. The presence of her primary care physician in addition, however, proved essential in helping her feel comfortable with her options. Primary care physicians are charged with taking care of the whole patient, a-fib, pain, tears and all. So when it became Dr. Gold’s turn to offer his input, he took a step back and considered her quality of life and her priorities. He helped her to sort through the risk calculators, EKG results and medication side effects to reveal what was really causing her the most distress each day and keeping her up at night. It was not her cardiac issues. It was her pain. Perhaps, he advised, we should address this issue first and then reconsider starting blood thinners in the future.
I would argue that any primary care physician would want this opportunity, the chance to sit down with his or her patient and another member of the healthcare team for one hour and determine what is really best for the patient at a given point in time. The problem is finding that hour amidst the multitude of patient visits, phone calls, notes, prior authorizations and EMR notifications. This time is what Dr. Gold offers his patients, and I believe that this single visit demonstrates how essential that time can be.
Tufts 3rd Year Medical Student
Employers and Direct Primary Care: A No-Brainer!

Not surprisingly, recent studies have shown a broad value proposition that links workplace health and well-being to favorable business performance. So why don’t more employers invest in programs that promote healthy employees? Expense is one glaring reason! Employers, both large and small, are being crushed by the rising cost of providing insurance benefits to their employees. Most employers address this growing cost by shifting it to their employees in the way of increased premiums, higher deductibles or higher co-pays. There is a cost effective solution and this solution is Direct Primary Care.
With Direct Primary Care, employers pay a fixed amount for all primary care services. This removes the guessing game on how much money will be spent on claims filed by employees. Direct Primary Care can be inserted into the overall health insurance plan offered to employees and ultimately control downstream costs. DPC, combined with an appropriate supplemental catastrophic plan, can save employers up to 40% on healthcare costs! This is all in accordance with the Affordable Care Act, so employers won’t get fined for non-compliance.
If saving money wasn’t enough to convince you, other perks for the employer include: decreased absenteeism, decreased workman’s comp claims, utilization of telemedicine to evaluate employees so they don’t leave early for doctors’ appointments or miss work altogether. Employees benefit too, as they receive same day appointments, a personal relationship with their physician, telemedicine/virtual visits, decreased out-of-pocket expenses, no more visits to urgent care centers.
Direct Primary Care physicians can be an employer’s most valuable ally as they search for ways to control healthcare costs, while simultaneously offering their employees the highest quality of care. Check out this article http://www.directdoctors.org/blog/direct-primary-care-a-solution-for-small-businesses to learn more.
If you are a business owner or know a business owner call us at 781-842-3961 to start saving money!
Why Are We Paying So Much Money For Health Insurance When We Still Can’t Afford Care?

The Boston Globe published an article on March 23, 2016 titled Even With Insurance, Mass Residents Often Can’t Afford Healthcare and I can’t even begin to explain how true this is. They really hit the nail on the head with this topic! Being a young adult, I can completely relate to what it’s like to not be able to afford health insurance. Not until last year did I really begin to understand how expensive health insurance really is. I started working for a big company which offered “the best” health insurance (no need to mention names). I was so excited to think I had this ‘top of the line’ health insurance. It was all great until of course, I made my first visit to the ER. With a very expensive co-pay, high deductible, and multiple bills later, I realized how unaffordable healthcare truly is. Just as this article states, having health insurance doesn’t necessarily mean you can afford care. I immediately noticed- yes, I finally have “great” health insurance, but does it even matter when I can’t afford to go to the doctor? With the statistics from the survey BCBS conducted, clearly I’m not the only one in the same boat. As mentioned in the article “43% of people said in 2015 health care and costs had caused problems for them and their families, including 19% who went without needed care as a result.” How crazy is it that almost 50% of the people surveyed have issues with health care costs?! That’s a huge percentage, which includes me, and possibly you too. We already have so many bills to pay and stress about, healthcare really shouldn’t be one of them. Another thing I noticed from the article are the comments being posted. So many people are complaining about this issue, yet they don’t want to do a single thing about it or, perhaps, they don’t know of other options out there. I think it’s time we start doing our research as healthcare consumers and see what other options we have out there!
This article really struck a chord with me, especially now knowing about Direct Primary Care and really understanding what it is. I wish I would have known about DPC earlier, or even know DPC was an option. Of course we do still need health insurance, but why not choose DPC for our primary care needs? This way we don’t have to deal with co-pays or high deductibles from our health insurance, not to mention getting more personalized care, appointments in a reasonable amount of time and honestly, a real connection with your doctor. Why wouldn’t you want a real connection with your doctor?! They are the ones who are dealing with a big part of your life; your health. The article from the Boston Globe should really relate to many of us, and also be an eye opener. With the results from the survey by BCBS, we can’t deny health insurance is way too expensive and we just aren’t receiving the best care for the amount we are paying. Instead, we end up with a huge headache because of very high bills and often poor to mediocre healthcare.
Written by Jessica Leon, Administrative Assistant; Gold Direct Care
Opiates: A Painful Topic For Everyone
Todays Boston Globe has an article regarding physician prescribing of opiates to patients that have already experienced an overdose Opiate Prescribing to Patients With OD History. Between the documentary that HBO aired last night regarding the opiate crisis on Cape Cod and this article from today, I felt that as a primary care physician and as a resident of a seemingly “white-picket fence” suburb of Boston that has experienced its own opiate epidemic with the loss of too many good people- many of them kids-to this illness, it was worth commenting on. Many of these kids and young adults I knew and even played street hockey with as a kid. Others I did not know at all, but I can feel the loss when something like this happens.
I am not an Addiction Specialist or a Psychiatrist but as a Family Physician we do often deal with these issues and are usually the front door to the healthcare system. I have treated many patients that struggle with the disease of addiction and it is an extremely complex disease that is extremely difficult to cure and it usually coexists with other mental health diagnoses whether it be ADHD, major depression, anxiety disorders, bipolar disorder etc etc that add to the challenge. The hardest part of the disease to address initially is the denial. As a key cog in the wheels of this disease, denial is the toughest nut to crack. Just like any other chronic disease we treat, patients have to come to some degree of acceptance to move forward, and with addiction denial prevents this from happening easily. Sadly, we have no idea when that bridge of denial will be crossed and what the outlook on the other side looks like, but it needs to be crossed nonetheless.
I may be an idealist at heart and obviously have my biases, but I think one key solution to this epidemic is better primary care. People that struggle with the disease of addiction obviously need a multidisciplinary approach- one that includes doctors, nurses, social workers, counselors, addiction specialists etc- but they also need a primary care doctor that can help them navigate this messed up system, be the teams quarterback, and most importantly know them and treat them as a human being rather than just a “disease”. We need to ask the hard questions such as “with all the stories and news out there on this issue, what drove you to take that pill that started it all? what support system if any do you have? how can WE help YOU get healed? How do we as a community band together to educate and support our kids in a nonjudgmental supportive way? What are WE as a community doing wrong?” It isn’t all about the actual drug or the patient and the choices they have made. Its an US issue because it could be any of our friends, family members, or children that can succumb to this disease. And I don’t know about you but aren’t you tired of reading these obituaries week after week?
Our primary care system and mental health system need an overhaul for many reasons, but this epidemic is a big one. All patients of all socioeconomic backgrounds that struggle with this awful illness deserve better than 15 minute visits. They deserve better than more pills thrown at them. They deserve a relationship that is based on trust, care, and respect. What if the doctors that were studied in the aforementioned article had time to research records and databases during these visits? What if they actually had time to call other members of the patients care team? What if they had time to discuss the risks, benefits, and alternative options for pain management with their patients with appropriate, close followup and communication? I can personally attest to the fact working in the Direct Primary Care model has allowed me to treat patients with addiction 100% better. I have the time to listen, call other resources if needed, and followup frequently by phone or email. I am by no means perfect and do not always have success sadly. Yet there is one thing that DPC has allowed me to show the patient who struggles with addiction that all the Continuing Medical Education and seminars in the world do not even touch on and that is……that I too am an imperfect human being, that I do care, and that there is hope. I know this idealistic view will not solve the whole crisis, but maybe infusing some humanity towards these patients is a good start towards helping them heal and live a healthy life? What we are doing certainly is not enough and to me that is unacceptable.