Tag: doctor
Why DPC IS The Answer!
Yesterday Dr. Edmond Weisbart wrote this article for Family Practice Management (http://www.aafp.org/fpm/2016/0900/p10.html#commenting) which we posted on our Facebook page last night. He basically gives reasons why he feels DPC is not a solution to our healthcare crisis. I took the liberty of writing the below rebuttal which I have since emailed to their editorial staff for publication as well as a medical blog called www.KevinMD.com. I truly hope you will read this, and if you agree with my arguments, help us DPC doctors across the country that are trying to fight for you, our patients, and speak up to everyone. Send letters to your congressmen and congresswomen. Send it to our governor. Share it on social media. WE- patients and doctors- need to fix this as people are paying more for healthcare than their mortgages and getting less and less in return.
September 14, 2016
I am writing this letter on behalf of my fellow DPC colleagues in response to the Opinion piece by Edmond S. Weisbart, MD, CPE, FAAFP from your September-October issue titled “Is Direct Primary Care the Solution to Our Health Care Crisis?” I will be so bold as to answer Dr. Weisbarts questions with an affirmative “yes” and will try to respond to each of his bullet points. For further reading that is excellently done and supported by fact please refer to Dr. Phil Eskews piece “In Defense of Primary Care.” (http://www.aafp.org/fpm/2016/0900/p12.html)
- DPCs exacerbate the growing physician shortage: No Dr. Weisbart, plain and simply our current system is exacerbating the shortage of physicians. People who choose to go into a primary care field want to care for patients and not be burdened with an excess amount of bureaucracy that prevents them from following their oath to provide said care. One could argue that many physicians taking administrative jobs, such as a CMO of a pharmacy company, could also be contributing to the “care” shortage and access problem. Maybe we should stop doing that? And having a panel size of 2,300 patient is a good thing? If our system continues down its current path our primary care will be nothing more than an Urgent Care clinic.
- DPC’s are essentially unregulated insurance, capitating physicians and removing vital protections: Where do i begin with this one? Insurance by definition is to protect people against major financial loss for major unexpected events i.e. life insurance, car insurance, home insurance etc. Primary care is not an insurable event, as everyone needs it and should have it. Primary care is actually highly affordable, but has been made expensive BECAUSE we insure it. And the difference between captivated plans from an HMO and DPC is that there is NO THIRD PARTY determining the capitated value for the primary care services. The sole value determinant is the actual patient. What a novel concept that we have completely failed to see since third party payers have stepped into primary care. You know? To help weed out those greedy PCP’s- compared to the affordable premiums people (many with chronic disease) are paying to to carry, only to have 3,000-6000 deductibles and zero transparency on pricing for outpatient services in the third party system. Plus, if providing your technical skills and knowledge for a set monthly fee is unethical or illegal, then why can lawyers, accountants, etc do this everyday? And as far as your HIPAA concern, in true DPC guess who has access to the patients file? me and the patient!. Thats it. No one else unless its the patients choice. Can’t get more private than that can you? If I do sell patients info to vendors I am pretty sure my state BORIM and the exodus of my patients will regulate me sufficiently thank you very much. No other third party or acronym needed for that.
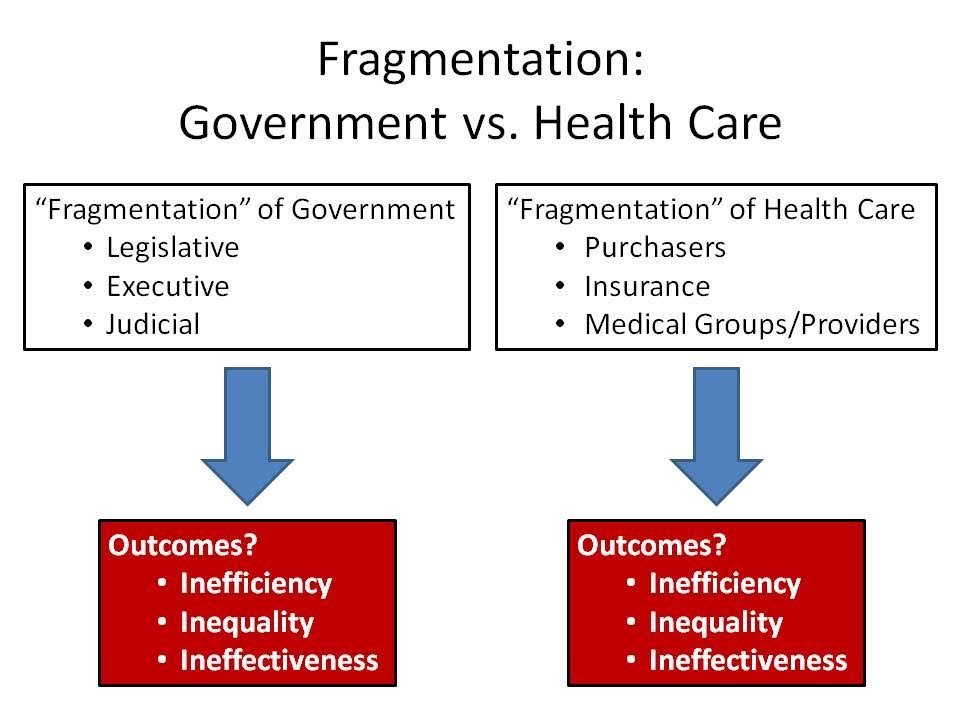
- DPC relies on an erosion of medical benefits: Lets look at your first sentence. The under-utilization due to HDHPs is actually due to the fact that people have no access to transparent care due to this third party payment cartel we have abided by for decades. Secondly, the current system is THE “hardship to patients” because it is an over regulated Gordian knot. DPC is accessible, affordable, and transparent with discounted pricing on imaging, labs, and meds in most states- i.e. those that allow dispensing. We actually help patients navigate this nebulous system, save them money, and yes, get them to specialists when needed with less fragmentation of care through better communication with said specialists. The only thing that makes specialty referrals difficult is the insane red tape that already exists (ie HMO patients needing an “in-network PCP” as their gatekeeper. So much for being “locked in” to something right?) We also use services (at no extra cost to patient I may add) like RubiconMD that reduce a lot of unnecessary speciality referrals that the 8 minute visits in our current system exacerbate. Also, many specialists will also see patients for a cash price if uninsured or underinsured. Thirdly, as far as employer plans go, the employers allow their employees to choose their own physician. DPC is offered as an option, not a mandate. They still have insurance, albeit with copays and deductibles, if they choose to have a PCP in the 3rd party system. So that statement is completely erroneous.
- DPCs exacerbate disparities in care: I will simply ask this in rebuttal- instead of citing studies. Have you actually visited a DPC practice and spoken to the patients that are members? Yes, the wealthy can afford anything. But what about all of those people you mentioned in paragraph 2 of section 3? A 90 dollar lipid panel at a hospital based lab is better for a blue-collar patient/family than a 75-95 dollar a month primary care medical home with no copays/deductibles and a 6 dollar lipid panel? Do the math. And as far as your inference to “cherry picking” patients with chronic diseases such as diabetes- that is just completely false and presumptuous. If anything, myself and my colleagues have many patients whom the current system has completely failed. But again, maybe you should actually speak with some DPC patients? Many of us actually have Medicaid patients. Being “insured” does not equate to actually receiving “care.” I will even provide charity care for those truly in need. Maybe policymakers and Medicaid administrators would actually work with us to make the model more accessible to Medicaid patients? Maybe the government could give those patients a voucher card for DPC no different than they do for food stamps etc?
The bottom line Dr. Weisbart is that nothing we have done or continue to do with this top down approach to fix our broken healthcare system is working. We have many administrators, policymakers, and CEOs telling us how to fix this and plugging fingers in the dyke that is ready to collapse as people pay more for insurance than they do their mortgage! So why don’t we try listening to the doctors and patients that have become the blips in the matrix on how to fix this mess for a change? The best solution to a complex problem is often the simplest. Remember Occams razor?
Sincerely yours,
Jeffrey S Gold MD
Owner/CEO Gold Direct Care PC
123 Pleasant St Suite 105
Marblehead MA 01945
DPC Coalition Steering Committee Member
Defragmentation of Care- PCP and Specialist Combined Visit ( A Medical Students Take)
When was the last time your PCP accompanied you to a specialist visit? Never? Same here. That’s actually not entirely surprising in today’s healthcare environment, given the demands placed on healthcare providers and primary care physicians in particular. But last week, I had the opportunity to be a part of such a visit.
I’m a medical student on my family medicine clerkship with Dr. Gold, and on his schedule this day was a cardiology visit for one of our 78 year-old patients. In the afternoon, we drove to meet her at the cardiologist’s office. She had recently had an episode of atrial fibrillation picked up by her pacemaker, and at this appointment, we would discuss the possibility of starting her on blood thinners. The cardiologist thoroughly explained the algorithms that guide decision-making for the treatment of new a-fib, along with the risks and benefits of blood thinners. He concluded by saying that, while he slightly favored starting the medication, he would leave the decision to our patient. As she took a moment to take in this information, her eyes began to well up. Amidst her tears, she explained that having to add yet another medication to her regimen or the thought of a stroke or going into a-fib again or bleeding from a fall was all too overwhelming to process.
The situation was complicated further by our patient’s chronic pain, which she experiences as a burning sensation across her lower chest. It has been treated with varying success for many years, and she was soon visiting a pain clinic for further assessment. So how was she to decide given these circumstances? The cardiologist offered expertise focused on giving her the best possible care for her cardiovascular health and went on to reassure her that the pain was not cardiac in origin. The presence of her primary care physician in addition, however, proved essential in helping her feel comfortable with her options. Primary care physicians are charged with taking care of the whole patient, a-fib, pain, tears and all. So when it became Dr. Gold’s turn to offer his input, he took a step back and considered her quality of life and her priorities. He helped her to sort through the risk calculators, EKG results and medication side effects to reveal what was really causing her the most distress each day and keeping her up at night. It was not her cardiac issues. It was her pain. Perhaps, he advised, we should address this issue first and then reconsider starting blood thinners in the future.
I would argue that any primary care physician would want this opportunity, the chance to sit down with his or her patient and another member of the healthcare team for one hour and determine what is really best for the patient at a given point in time. The problem is finding that hour amidst the multitude of patient visits, phone calls, notes, prior authorizations and EMR notifications. This time is what Dr. Gold offers his patients, and I believe that this single visit demonstrates how essential that time can be.
Tufts 3rd Year Medical Student
Open Enrollment: What to do next
For all of you who are in the enrollment period for employer-based insurance, including town employees, we can help answer your many questions. We offer free one hour consultations to help look over your insurance benefits. We also show you how Gold Direct Care can complement your insurance in a way which accomplishes two main goals:
1) Provide you with better access to primary care (AKA better quality care) with a doctor that is available to you when you need them. Appointments guaranteed within 24 hours and no insurance hassles.
2) Lower your cost. By combining our aged-based monthly fee with a lower premium/higher deductible plan we can get you to either break even for better value or, best case scenario, we can save you money all the while keeping you protected medically and financially.
We understand how complex insurance options can be. We are here to help you become a better consumer and navigate these complexities, so you and your family are protected; all the while getting the best value for their dollar. Please contact us for any inquires and to set up a time to talk at info@golddirectcare.com or 781-842-3961.
We also have knowledgeable insurance consultants as well whom we can direct you to if needed.
Here is an article with great examples if you would like to learn more: What Really Happens When You Cut The Red Tape